Immunotherapy (therapy)
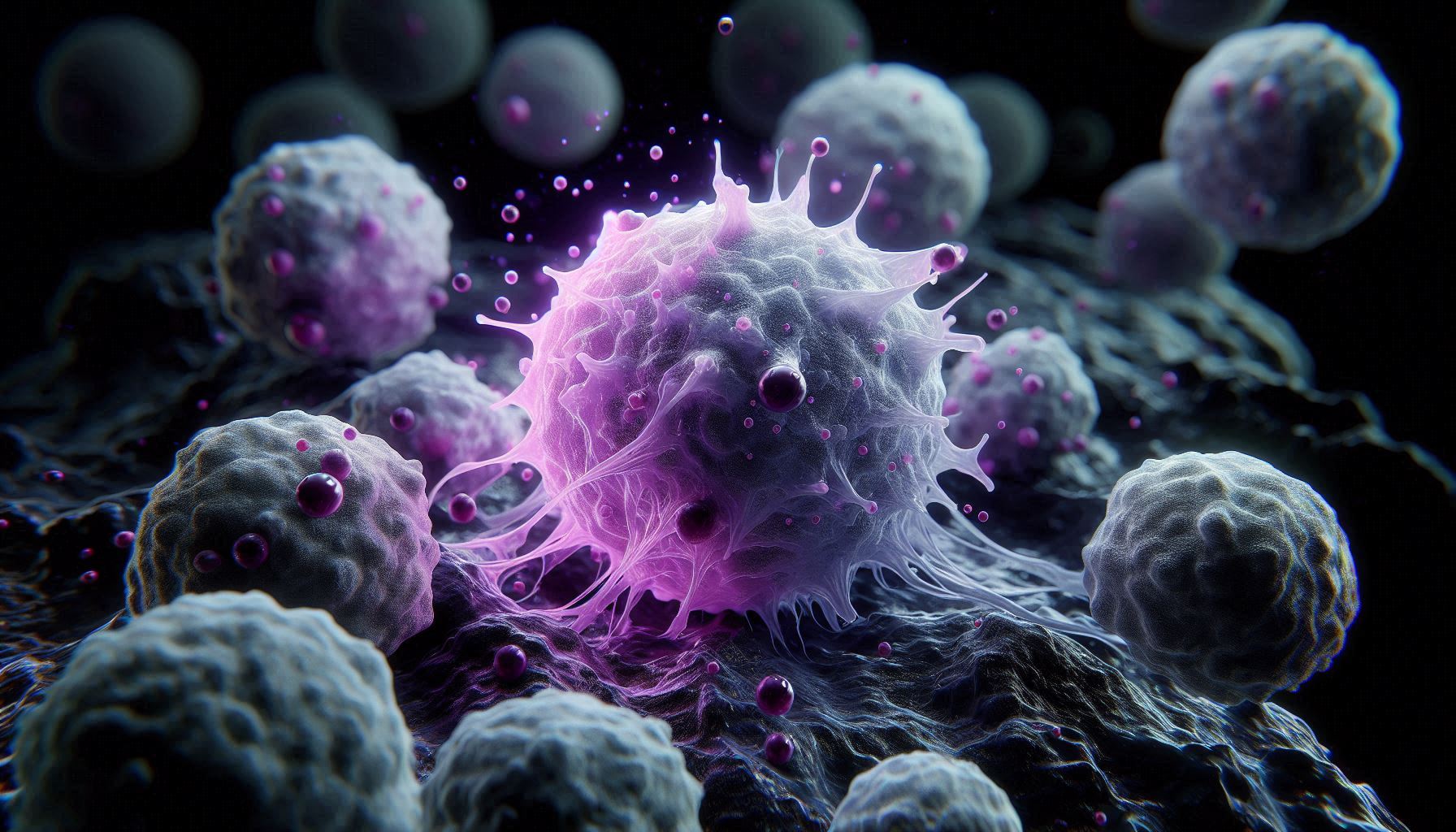
Immunotherapy has transformed cancer treatment, yet solid tumors remain a major challenge. Two cutting-edge projects, CAR-MAC and PRODIGY, aim to overcome these limitations by developing engineered macrophage-based immunotherapy and targeting DNA damage response (DDR) pathways. These strategies enhance immune infiltration, improve tumor recognition, and provide new therapeutic avenues for cancers such as breast cancer and glioblastoma.
The CAR-MAC and PRODIGY projects represent major advancements in immunotherapy by combining cellular engineering and proteogenomic innovations. CAR-MAC therapy enhances immune targeting of solid tumors, while PRODIGY deciphers DDR pathways to optimize therapeutic strategies. Together, they pave the way for highly personalized and efficient cancer treatments, bridging technological and therapeutic innovations to revolutionize the fight against cancer.
Key Research Axes
CAR-MAC – Advancing Macrophage-Based Immunotherapy
CAR-MAC therapy involves engineering macrophages with chimeric antigen receptors (CARs) to recognize and destroy cancer cells. Unlike CAR-T cells, macrophages can penetrate solid tumors and reprogram the tumor microenvironment, making them a promising alternative for hard-to-treat cancers.
Key Objectives
- Develop HER2-targeting CAR-MACs for breast cancer treatment.
- Identify and validate alternative proteins (AltProts) as new tumor antigens for personalized immunotherapy.
- Create light-switchable CAR-MACs (LS CAR-MAC) to mitigate treatment toxicity.
- Establish a synthetic antigen system to enhance universal CAR therapy.
Innovations and Progress
- HER2 CAR-MAC therapy: Successfully developed and validated against HER2+ breast cancer cells, showing enhanced phagocytic activity when combined with PC inhibition.
- Proteogenomic discovery of novel antigens: Advanced sequencing and proteomics techniques identify unique tumor markers from patient biopsies.
- Ex vivo and in vivo testing: Breast cancer tumoroids and bioprinted tumor models (BREASTMO) allow preclinical evaluation of CAR-MAC efficacy before clinical trials at CHU Lille.
- Synthetic antigen strategy:
- Development of tumor cell “tagging” using foreign antigens (β-galactosidase, mCherry, hemagglutinin).
- Delivery via adeno-associated viruses (AAV) for glioblastoma therapy.
- Preclinical testing on companion dogs with inoperable glioblastoma.
- Light-switchable CAR-MACs (LS CAR-MACs): Using photolyase domains (CRY2/CIB1), immune activation can be controlled with light exposure at 488 nm, offering a safer and more precise treatment option.
PRODIGY – Enhancing Immunotherapy Through DDR Targeting
Tumor cells rely on DNA damage response (DDR) mechanisms to survive genomic instability. Targeting DDR pathways can increase tumor vulnerability and enhance immune system activation. PRODIGY aims to uncover DDR-based therapeutic hallmarks to potentiate immunotherapies, particularly in glioblastoma (GBM).
Key Objectives
- Identify DDR proteoforms (Pf) to personalize DDR-targeting therapies.
- Develop a Proteoform-Proximity Labeling (Pf-PL) approach to study DDR protein interactions and post-translational modifications (PTMs).
- Use DDR inhibition to boost immunotherapy efficiency by promoting immune infiltration via the cGAS-STING pathway.
- Refine tumor protein interaction networks using advanced protein footprinting and mass spectrometry techniques.
Innovations and Progress
- DDR proteoform discovery: Using TurboID proximity labeling, PRODIGY maps protein modifications and their role in DDR checkpoint activation.
- PTM-specific protein interaction analysis:
- Pf-PL technology identifies DDR protein interactors based on their modification state.
- Split-TurboID & light-activated crosslinking enhance specificity in mapping transient DDR interactions.
- Protein interface mapping for drug discovery:
- Hydrogen-deuterium exchange (HDX), carbene footprinting, and in-cell Fast Photochemical Oxidation of Proteins (IC-FPOP) identify druggable protein interfaces.
- These findings provide novel DDR-based targets for therapeutic intervention.
- DDR inhibition as an immunotherapy enhancer: Blocking specific DDR pathways increases tumor immunogenicity, enabling better immune infiltration and synergy with CAR-MAC therapy.